Whether you have good oral hygiene or a less-than-stellar smile, there may come a time in your life when you need to go under the knife for oral surgery. Modern oral treatments might remedy your mouth issues after healing the right way, but these procedures can also cause painful dry socket symptoms.
Even the most common kinds of dental procedures can be the cause of your painful dry sockets, such as:
- Wisdom tooth extraction or tooth removal
- Maxillofacial surgery (cleft palettes, jaw reconstruction, etc.)
- Root canals and crowns
- Cosmetic or reconstructive dental implantations
Pain at the extraction site or in your tooth socket can be excruciating, so stay vigilant and look for symptoms of dry socket formation. Patients who hesitate to seek prompt treatment from their dentist after developing a dry socket risk dangerous infection and further issues down the line.
Keep reading to learn more about dealing with your dry socket problem with minimal pain.
What Is a Dry Socket?
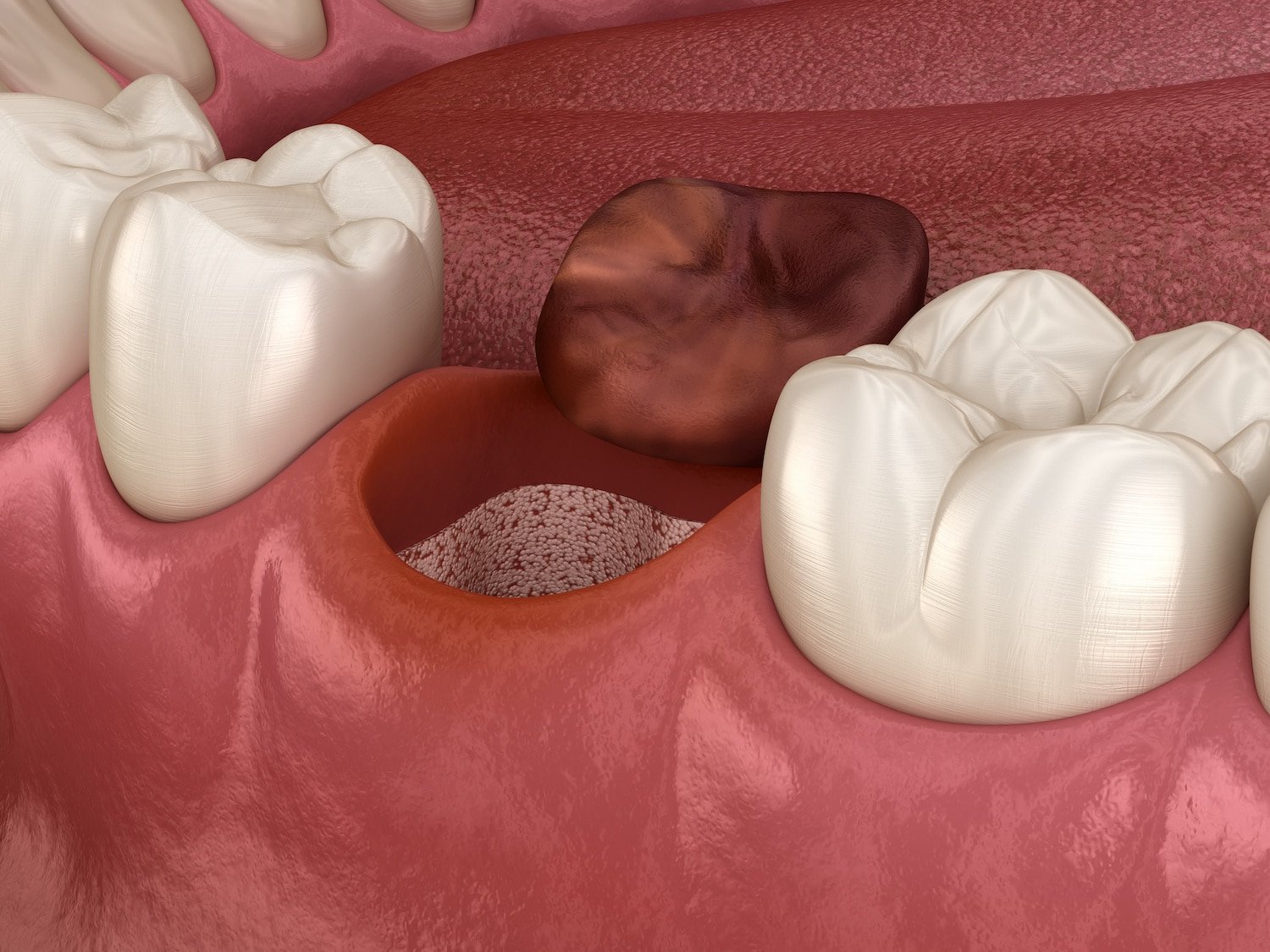
If you have a tooth extraction or other oral procedure coming up, you might be concerned about experiencing the infamous and extremely painful symptoms of a dry socket. Dry sockets – or alveolar osteitis – occur when patients accidentally dislodge the blood clot that forms in empty sockets at an extraction site, potentially exposing soft tissue, bone, and nerves.
Certain people are prone to developing unavoidable pain at the extraction site due to predisposing factors, while others are at an increased risk for a dry socket issue from ignoring their dentist’s instructions. These are the patients that choose to pursue activities that disrupt the healing process in affected areas, often causing painful dry sockets.
While it’s not the most common complication these days, you’re most likely to develop dry socket pain from:
- Poor oral hygiene
- Lack of preventative care
- Drinking alcohol, smoking, and using chewing tobacco products
- Strenuous physical activity
- Sucking liquid through a straw
- Chewing hard foods
- Exposure to extreme hot and cold temperatures (food/drink)
- Underlying health conditions and other risk factors
Your Blood Clot Is Your Best Friend 🩸👩🏼🤝👩🏽
The blood clot that forms provides a layer of protection from outside bacteria while also helping to promote healing inside your mouth. If that blood clot becomes dislodged, you’re more susceptible to developing dry socket symptoms.
Preparing for a Tooth Extraction

Any kind of oral procedure can seem scary, especially since there’s a slight risk of dry socket development, but don’t worry. You can take several steps or even seek preventative dental services to ensure your healing process goes smoothly. Make sure to:
- Complete your initial consultation with a reputable dentist or oral surgeon in your area. Learn how to find the right provider in this helpful guide. 👨⚕️🦷
- Disclose all of your current prescription medications and family medical history. 🧬💊
- Ask your dentist or oral surgeon if any antibiotics are required before or after the tooth extraction to help avoid infections and ensure proper healing. 🚫🦠
- Before the procedure, stock up on plenty of soft foods such as ice cream and yogurt since you should only eat soft foods after tooth extractions to avoid a dry socket. 🍦🍧
- Try your best to quit smoking (or at least be able to cut it out for a couple of days) before your procedure. 🚭🚭
- Consider the best methods of aftercare and pain management to promote healing, relieve pain, and minimize the risk of dry socket formation, whether that’s buying over-the-counter medications, preemptively freezing cold packs, or calling on a spouse or friend to provide proper care as you rest and heal. 🩹🩺
Taking time to prepare before a tooth extraction can help prevent dry socket issues after your procedure.
8 Symptoms of Dry Sockets That’ll Send You Back to the Dentist
If the protective blood clot in your mouth becomes dislodged for any reason, a dry socket may form – and those never feel nice. Don’t be afraid to seek dry socket treatment if you notice some common symptoms, such as:
1.) Severe Pain
Whether it’s a difficult tooth extraction or a routine procedure, no patient is immune from experiencing the excruciating pain of a dry socket. Debilitating pain is the primary symptom of a dry socket, and although oral surgeries are always uncomfortable, it’s worsening pain that will likely be the first sign you notice.

2.) Loose or Missing Blood Clot
As we already touched on above, clotting is required in the empty tooth socket to ensure proper healing after having a tooth extracted. When a clot gets dislodged, you’re like to develop dry sockets in the tooth extraction site.
3.) Exposed Bone
When blood clots get dislodged, the bone in your gum can get exposed. Examine your mouth with a flashlight and mirror to make sure your medicated dressing is in place and no underlying bone is visible in your empty socket.
4.) Mouth and Gum Sensitivity
If bones and nerves become exposed, you can become extremely sensitive to certain things, especially at the extraction site. Hot and cold food and drinks, or even the slightest touch, can send shooting pain through your mouth.

5.) Bad Breath
If bacteria gets into your exposed socket, there’s a chance for infections to develop. Mouth infections often lead to bad breath, which is a big indicator you have a dry socket.
6.) Excessive Bleeding
If you notice your medicated dressing repeatedly (and increasingly) becoming soaked with blood, you might have a dry socket. Patients with particular prescriptions should ensure there’s no risk for poor blood clotting to prevent dry socket problems.
Examples of medications to watch out for when having a tooth extraction include:
- Oral contraceptives or birth control pills
- Anticoagulants/blood thinners (Warfarin, Heparin, etc.)
- Antiplatelet medications (i.e., Aspirin, Entrophen)
- Anti-inflammatory drugs like Ibuprofen
Drug interactions are nothing to ever mess around with, even if you’re having a routine wisdom teeth removal. Talk with your dentist or oral surgeon about any current prescriptions and have all possible contraindications clinically reviewed to ensure everything in your system can mix safely before surgery. This way, you won’t risk excessive bleeding at the surgical site that leads to a dry socket.
7.) Unpleasant Taste
Another common symptom of a dry socket is a bad or sour taste in your mouth. This can be one of the first signs of infection, so don’t let that smell linger without taking swift action. Swish warm salt water or a dentist-recommended rinse in your mouth gently before getting on the books at your local dental office.
8.) Bacterial Contamination
If you’ve noticed a foul smell or taste inside your mouth, the bacterial infection has likely already taken hold. Signs of bacteria, such as white, puss-like growths, indicate it’s time to give your dentist’s office a call because infections like sepsis can be serious or even life-threatening.

Stop Suffering From Dry Sockets
Even with the best preventative dental services in Minnesota and intensive preparations prior to your procedure, there’s no surefire way to stop dry socket problems and ease pain after an extraction by yourself – but you’re not alone.
If you’re suffering from symptoms of dry socket post-op, stop agonizing in silence. Ask for help from the expert dental team at Wayzata Dental. We can’t wait to meet you!
FAQ
How do I know if I gave myself a dry socket?
Severe pain after tooth extraction may indicate dry socket.
When is dry socket no longer a risk?
Dry socket risk decreases significantly after a week.
Will a dry socket heal on its own?
No, seeking dental treatment is necessary for healing.


